The purpose of this blog is to highlight what women might experience after giving birth and entering menopause. These are two major life changes for women and not enough information about the impacts of these changes on sexual function. What is normal? What is common? What can I do?
First, let’s define sexual health, The World Health Organization describes sexual health as, “a state of physical, emotional, mental and social well-being related to sexuality; it is not merely the absence of disease, dysfunction or infirmity (physical or mental weakness)” (1). Simply put a healthy sex life is not just the absence of illness or dysfunction. So what might be some of the causes of sexual dysfunction in women?
So, sexual dysfunction is a general umbrella term that includes sexual pain disorders, hypoactive sexual desire disorder and arousal and orgasmic disorders (1), which in layman’s terms means painful sex, lack of desire and difficulty becoming aroused or orgasming.
About 40% of women experience sexual dysfunction after giving birth (1).
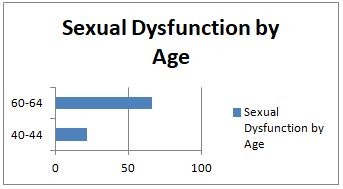
About 51.3% of women experience sexual dysfunction in the menopausal phase (2).
The graph below shows the percent of women experiencing sexual dysfunction in the peri-menopausal-menopausal phase.
Sexual dysfunction is more common than you think. Of course it is very personal so it’s likely that many women aren’t sharing their troubles with healthcare providers, let alone friends/family. It may be common but it doesn’t necessarily mean it is normal.
What are some reasons women experience sexual dysfunction after pregnancy/birth?
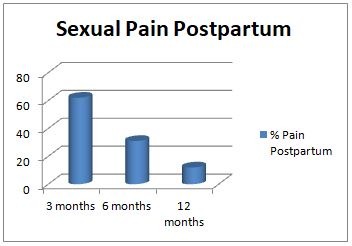
The most common reason for women not to return to sex right after a baby is pain. One study of 796 first time moms revealed that 62% experienced pain at 3 months, 31% at 6 months and 12% at 12 months (1). (see graph below).
Women were 80% more likely to experience pain with a second degree tear and 270% more likely with a third or fourth degree tear (1).
Birthing a baby can cause trauma to the muscles and tissue around the vaginal opening. Once healed there may be scar tissue, tension and tightness, which can cause pain. There is something you can do about it however. Pelvic floor physiotherapy can help address this problem and set you up on a plan to return to more pleasurable sexual experiences.
Low sexual desire is reported by about 53% of women at 3 months postpartum compared to 37% at 6 months post partum (1). Most studies find that desire improves over time and was mostly impacted by changes in body image, mother’s mental health and the status of the martial relationship (1). Many women report that the physical changes to their body following childbirth makes them feel less attractive (3) and that they were anxious about the looseness of their vagina (3).
Breast-feeding women versus non-breastfeeding women appear to return to sex much later. One study of 25 first time moms found decreases in the levels of testosterone and androstenedione, which are responsible for increased sex drive. This is supported by another study of 576 women who reported low or no arousal during the time of breastfeeding (1).
Other factors reported by women are the changes in priorities. Whenever they get spare time, they just want to relax and read or sleep (3). The demands of the child often leave the mother fatigued and desiring alone, quiet time versus engaging in sex (3). When women were asked about their low desire, the most common reasons reported were, tiredness, breast-feeding, lack of time and concerns over vaginal damage from delivery (3).
What about in menopausal women? Is it hormones or age that impacts sexual experiences?
Peri-menopausal and menopausal women most often report sexual pain and low desire for sex.
One study of 438 Australian women between the ages 45-55 that were still menstruating sought to find an answer- is it age or hormones- what they found in the study is that it is both. As these women aged, sexual responsiveness decreased (4). Sexual frequency and libido was significantly less for postmenopausal women suggesting a hormonal role and how decreased hormones can impact pain with intercourse (4). Hot flashes did not impact sexual experience directly but had other impacts on health quality of life, which indirectly impacts sexual functioning (4).
Let’s look at hormones first. Estrogen’s role in arousal is vaginal lubrication and vasocongestion, which means swelling of tissues, i.e blood flow (5). In the transition to menopause, estrogen levels drop and women more commonly complain about dryness, thinning of the vaginal walls and blood flow changes which can lead to pain with intercourse. When it hurts to have sex, our motivation to have sex is going to be impacted.
Testosterone plays a role in sex drive and libido. Women who are more “stressed” generally have lower amounts of hormones, including testosterone and women who had a hysterectomy and their ovaries removed will have fifty percent less testosterone (6).
Another hormone of interest is cortisol, which is a hormone produced by the adrenal glands, along with DHEA, which is a main building block for estrogen and testosterone (5, 6). Higher levels of cortisol prior to arousal may actually inhibit or make you less likely to engage in sexual activities (5). However, it is true that having sex does decreases the levels of coritsol, i.e we feel less stressed after sex (5).
There are a number of other considerations to take into account when sex drive is low. Menopause is a time of transition and change. Our bodies are changing and so are other psychosocial factors, for example, whether we have a partner, are single or been with someone for a long time (4). The age and health of our partner and their sexual functioning impacts a women’s sexual experiences (4). How we feel towards our partners and the level of sexual activity previously. Other factors include, employment satisfaction, social class, level of education, access to health providers, personality, negative attitudes towards self or partner and actual physical and mental health (4).
There is a lot more going on for new moms and women entering the menopausal phase. Can pelvic floor physiotherapist help alone? Maybe but likely no. As a pelvic floor physiotherapist I will be address the tissue dysfunction that may be present. I will do lots of education around healthy lifestyle, stress management, exercise and pain, but I cannot address the hormonal component.
Your Family Doctor or a Naturopathic Doctor can discuss hormones and what would be best for your situation.
Now we cannot forget about the mental, emotional and social factors going on during these times of change. Learning to cope, think different, interact with our feelings/emotions is best to explore with a trained professional that can guide you. This type of help can be provided by a qualified psychotherapist that is trained in emotional and cognitive behavioural therapies. They can help you explore all your thoughts and feelings in a safe environment without the fear of judgment.
So… to finish off the blog, we have an ask. We are looking for feedback. We have created a completely anonymous survey of 5 questions related to painful sexual experiences. No personal information will be collected. We are looking to find out what your challenges are and what resources/information would be most useful to you for overcoming the problem. Please visit www.ecophysio.com/survey to complete the survey.
Written By: Madelaine Golec PT, Pelvic Health Physiotherapist
